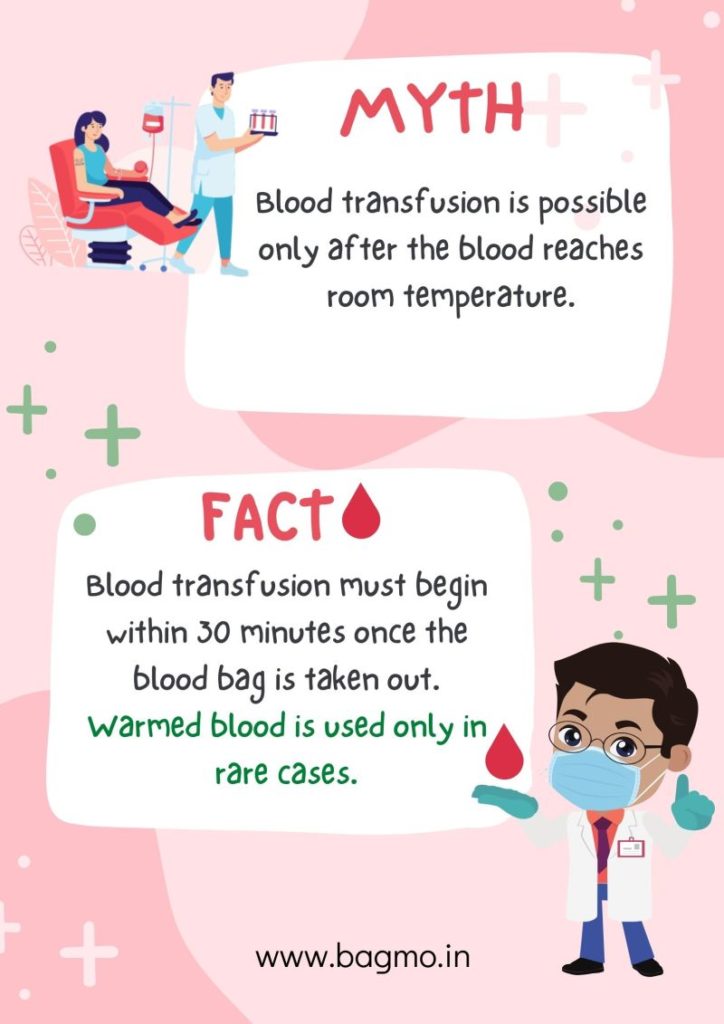
#Bloodtransfusion is possible without thawing #blood to room temperature. After taking a #bloodbag out of the refrigerator, it is mandatory to begin blood transfusion within 30 minutes. #Clinicaltransfusion guidelines approved by #WHO state that administering cold blood at slow rates does not affect the patient adversely. Hence, it is not mandatory to warm the blood.
However, we must thaw blood to room temperature for :
– exchange transfusion in infants
– patients with clinically significant agglutinins
– large volume rapid transfusion – flow rate more than 50ml/kg/hr for adults and above 15ml/kg/hr for children.
We must use only blood warmers for warming blood. Using hot water to warm cold blood will lead to hemolysis of RBC which is life-threatening upon transfusion. Once we take out a #bloodbag from a temperature-controlled storage environment, it is necessary to #transfuse it or return it, if not transfused within 30 minutes. If the blood bag is left out at room temperature for more than 30 minutes, the chance of bacteria contamination in the blood is more.
The #bloodbankmanagementsystem, #Bagmo, assists the staff at the blood bank to track the temperature and quality of individual blood bags. The #Bagmo#bloodbagmonitoringsystem alerts the staff if a blood bag is out of a BBR for 30 minutes or more. Hence, ensuring safe blood and reducing wastage.
References
1. World Health Organization. (2020). Clinical transfusion practice: guidelines for medical interns. Available at:https://www.who.nt/bloodsafety/transfusion_services/ClinicalTransfusionPracticeGuidelinesforMedicalInternsBangladesh. pdf. Accessed July, 2.
2. Brunskill, S., Thomas, S., Whitmore, E., McDonald, C. P., Dorée, C., Hopewell, S., … & Murphy, M. F. (2012). What is the maximum time that a unit of red blood cells can be safely left out of controlled temperature storage?. Transfusion medicine reviews, 26(3), 209-223.
